
What I Wish People Knew About Dementia
Wendy has released a second book, called 'What I Wish People Knew About Dementia', which looks at the many misconceptions people have about life with dementia.
Despite spending 20 years working for the NHS, where she would train nurses on how to roster staff, Wendy Mitchell admits the word ‘dementia’ had never entered her vocabulary. That changed on 31 July 2014, the day Wendy was told she had early-onset Alzheimer’s, aged 58.
Soon after her diagnosis, Wendy began writing a blog, Which me am I today?, which continues to diarise her experiences of what she calls her “new life” with dementia, and the process of adapting she’s undertaken with her two daughters.
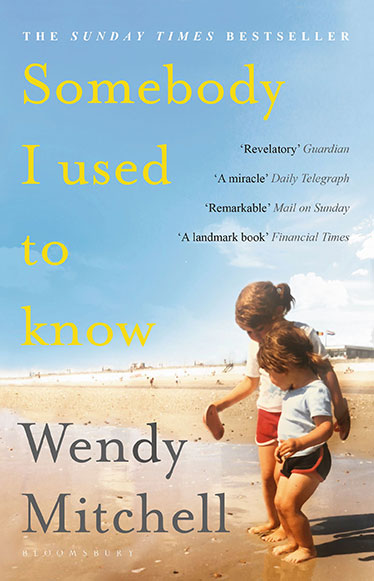
The blog also provided a valuable resource when it came time for Wendy to write her book (alongside author and journalist Anna Wharton), the Sunday Times Best Seller ‘Somebody I Used to Know’, which was released at the beginning of 2018 and has recently become available in paperback.
We sat down with Wendy to discuss her life before and after her diagnosis, as well as the writing of the book and what she thinks could be improved in how dementia is treated.
What is dementia?
Dementia isn't a consequence of growing old, but the risk of dementia increases with age. Most people who are affected by dementia are over 65, but there are many, like Wendy, who show symptoms when younger.
How would you describe your life before your diagnosis?
“I was a very, very work-orientated person – I suppose I was a workaholic. I adored my work and the NHS. I was also very fit and active; I used to run every other day. I didn’t smoke and I didn’t drink, so I didn’t fit the profile of what you imagine from someone being diagnosed with dementia.”
What did you know about dementia at that point?
“I was a bit like everyone else who thought it was only older people who got a diagnosis, so when I started having all of these strange symptoms, dementia never entered my head as a possible cause. I was thinking it was a brain tumour, or anything but dementia, so when it was mentioned in passing, that was a bolt from the blue.”
When did you begin to realise something was wrong?
“I used to be renowned for having a brilliant, encyclopaedic memory – I’d never forget anything – and suddenly it began to let me down very badly. I’d forget the simplest of words, or the names of people I’d worked with forever. Things just weren’t right, and then when I was out running, my legs and my brain weren’t talking to one another and I’d end up falling flat on my face. I knew that something wasn’t right.”
No one should underestimate the psychological effect that words have.
Having experienced symptoms for some time, how did you feel when you were diagnosed?
“It was obviously very devastating, but it was also, bizarrely, a relief because it finally gave me a name for what was happening to me – ending all the ifs, buts and maybes. I knew what I was dealing with and could plan my life around finding out as much as I could.”
What surprised you the most about the way in which clinicians deal with those with dementia?
“I think the biggest shortfall is the way clinicians deliver a diagnosis. No one should underestimate the psychological effect that words have. When I was given my diagnosis, the consultant had a sad look on her face, gave me a handshake and said, ‘Goodbye – there’s nothing we can do’. Imagine the psychological impact of being told that! I’m not downplaying it’s a bummer of a diagnosis, but if she’d instead said something like, ‘I’m afraid it is dementia, but think of it as the start of a different life. My mindset would have been so different when I left her office.”
How did you and your daughters adapt after your diagnosis?
“Once you’ve got your head around it, the most important thing you can do is to talk to your loved ones. Many people are afraid of hurting those closest to them, but if you speak openly about what you’re struggling with, they might be able to help you. It has to be two-way though; they have to tell you what they’re struggling with, so that you can explain what’s going on. Me and my daughters have realised the importance of this.”
What does a good day versus a bad day look like at this point?
“Let’s start with the bad day… I describe it as a fog descending on the brain. On those days little makes sense in the world around you and you can quite easily just curl up and wait for that fog to lift. Good days are days like this; all this travelling and talking to people [about the book] is like doing Sudoku because it exposes my brain to different environments, different people, different conversations – so it exercises my brain, even though it’s exhausting.”
What are you biggest frustrations with the way people interact with you as someone with dementia?
“If I’m with my daughters, people will speak to them instead of me, but my daughters are very good at saying, ‘Well why don’t you ask mum?’ When people hear the word ‘dementia’ they forget there’s a beginning and automatically think of the end. There’s so much life still to be lived, albeit differently and with lots of support. I always tell people they should never dwell on what they can’t do; I can’t drive or cook or do numerous other things, but there are lots of other things I can do, so I concentrate on those.”
How did the idea for writing a book come about?
“I’d been asked on numerous occasions to write a book and I kept telling people I couldn’t, because I’d end up writing the same thing on every page. Then the lovely Anna Wharton contacted me after she’d seen a film I made for a magazine. Her father had dementia when she was in her twenties, and she told me she wished she’d had a book at the time to understand what was happening, and believed we could write that book. I didn’t know her from Adam, so I had to really trust her, so we met in London one day. We immediately clicked and knew that we’d be able to find a way [to work]. Anna’s writer friends had said to her, ‘Are you mad to try and write a book with someone who finds it hard to remember?’ We had to find different methods to write together.”
What were those methods?
“Soon after diagnosis I started writing a daily blog, called ‘Which me am I today?’ Between then and now, my blog acts as my memory. If I didn’t write a daily blog then I’d forget whatever I’ve done by the next day. So for the last five years, [Anna and I] had my blog to go in chronological order. Before then, there was a period of 18 months while I was being diagnosed that I had very little recollection of, but by pure coincidence my daughter was keeping a diary during that time. And before then, I have a brilliant memory of everything that happened, so all of the pieces fitted together.”
Age UK Advice Line
Worried about a planned hospital stay? Looking for advice on choosing a care home that's right for you or a loved one? Our free, confidential, national phone service is open 8am-7pm, 365 days a year.
How did you and Anna work together on the book?
“Anna lives at the other end of the country, and I can’t use the phone anymore, so we actually wrote the book via WhatsApp and email. We’d spend all day WhatsApping each other, with Anna telling me which bit she wanted to write and me typing it. I can still type as if dementia has never entered my world because that part of my brain hasn’t broken. We’d have such a laugh because I’d say, ‘We must include this!’ and she’d say, ‘Nah, we did that last week’. It was also a very emotional time, because we were sharing each other’s lives for that year. We’re still very good friends now.”
Were there any things you were uncomfortable covering in the book?
“When [Anna and I] talked about end of life, at that point I hadn’t discussed it with my daughters. It was important that I had the conversation with my daughters first before I had the conversation with Anna and we wrote about it. I’m still a mum, first and foremost, so I wanted to make sure they were happy with the sections they were included in, so they would read those sections and either approve or not approve [them]. It was a very open process between us all.”
Pre-diagnosis, did you think you’d ever write a book?
“When I give talks, I often end by talking about ‘the advantages of dementia’, which causes some people to look horrified. I say it because I’m a glass-half-full person and have to see the positives to help me cope. I would never have written a book if I hadn’t been diagnosed with dementia, so all these positives are my way of coping with all cruel things that dementia throws at you.”
I like to think of a diagnosis as the beginning of a different life – one of adapting and support, and not one you’d have imagined whatsoever – but the start of a new life rather than the end of life.
In the book, you discuss leaving recordings for your daughters. How important do you think this process of leaving something behind is for those with dementia?
“Everyone is an individual, so when you meet one person with dementia, you’ve met only one person with dementia. Some things work for some people and don’t work for others. However, I always think that recording now, in whatever way is possible for you, is a legacy for your children and their children – and other generations. I find it a very comforting idea.”
What impact do you hope the book has on others?
“I hope that it gives them less fear about dementia. I like to think of a diagnosis as the beginning of a different life – one of adapting and support, and not one you’d have imagined whatsoever – but the start of a new life rather than the end of life. That helps people see it in a different perspective.”
What do you think can be done better in the treatment of dementia?
“We live in a medicalised world with dementia. I remember someone saying to me once that the clinician felt sad because she couldn’t do anything, but she didn’t think of what I could do for myself. I think there needs to be more social prescribing, rather than sticking to a purely medical model. When I got the diagnosis, so did my daughters, so the whole family needs education and support. The biggest support for me was peer support, listening to other people say ‘That happened to me’. You can feel very alone with a diagnosis of dementia, especially if you don’t know anyone else who has it, but listening to and laughing with other people with dementia is wonderful.”
Alzheimer's Society
Wendy is an ambassador for the charity, which campaigns and funds research to find a cure for dementia and supports people living with it today.

